In the realm of healthcare and social services, the concept of cultural competence has long been heralded as a cornerstone for providing effective care to diverse populations. However, recent research suggests that it's time to shift our focus towards cultural humility—a more dynamic and reflective approach that can significantly enhance therapeutic practices. This blog explores the findings of a pivotal research article titled "Rethinking Cultural Competence: Shifting to Cultural Humility" and offers practical insights for practitioners looking to improve their skills.
The Limitations of Cultural Competence
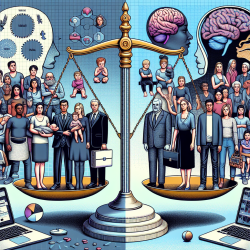
Cultural competence training has traditionally aimed to equip healthcare providers with knowledge about different cultures to improve communication and care delivery. However, this approach often risks stereotyping and othering patients by assuming a static set of cultural norms. The notion that one can become 'competent' in any culture is problematic, as it overlooks the fluid and intersectional nature of individual identities.
Research indicates that cultural competence training has limited effectiveness in improving patient satisfaction or health outcomes. This is partly due to its focus on increasing provider confidence rather than fostering genuine understanding and communication with patients from diverse backgrounds.
Embracing Cultural Humility
Cultural humility offers a promising alternative by emphasizing self-reflection, lifelong learning, and an appreciation for patients' lived experiences. Unlike cultural competence, which suggests mastery over cultural knowledge, cultural humility encourages practitioners to acknowledge their limitations and continuously learn from their interactions with patients.
This approach involves recognizing one's own biases and the power dynamics inherent in patient-provider relationships. By adopting a stance of openness and respect towards patients' perspectives, practitioners can foster more equitable and effective therapeutic partnerships.
Implementing Cultural Humility in Practice
- Self-Reflection: Practitioners should regularly assess their own beliefs, biases, and assumptions. Tools like Harvard University's Implicit Association Test can aid in this process.
- Lifelong Learning: Engage in continuous education about cultural dynamics and social determinants of health. This could involve attending workshops, webinars, or reading relevant literature.
- Patient-Centered Communication: Prioritize listening to patients' narratives and experiences. Adopt a less authoritative interviewing style to empower patients in sharing their stories.
- Power Sharing: Strive for balanced relationships with patients by valuing their expertise about their own lives and health contexts.
The New York State Training Model
A practical example of implementing cultural humility is the New York State Cultural and Structural Competence Training. This dual-component program integrates principles of cultural humility into practice through interactive sessions that emphasize self-awareness and patient engagement.
The training includes exercises that encourage participants to explore their own 'health habitus'—the ways culture influences their health behaviors—and engage in discussions about structural determinants of health. Such activities help deconstruct stereotypes and promote humility among practitioners.
Conclusion
The shift from cultural competence to cultural humility represents a necessary evolution in therapeutic practice. By embracing humility, practitioners can enhance their ability to provide truly patient-centered care that respects individual identities and experiences. As we move forward, it's crucial for healthcare providers to adopt this paradigm shift to address health disparities effectively.
To read the original research paper, please follow this link: Rethinking Cultural Competence: Shifting to Cultural Humility.