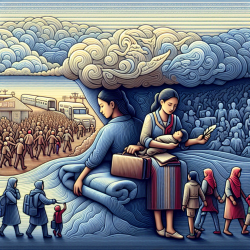
The COVID-19 pandemic has highlighted significant disparities in healthcare access and outcomes among communities of color in the United States. A recent study titled "Continuum of Trauma: Fear and Mistrust of Institutions in Communities of Color During the COVID-19 Pandemic" sheds light on the deep-seated fears and mistrust these communities hold towards public health institutions. This blog explores how practitioners can leverage these insights to improve their approach to care and encourage further research into culturally sensitive interventions.
The Impact of Historical, Cultural, and Social Trauma
The study identifies three main types of trauma affecting communities of color: historical trauma, cultural trauma, and social trauma. Historical trauma refers to the cumulative psychological and emotional injuries sustained over generations due to massive group trauma experiences. Cultural trauma involves ongoing assaults on a group's cultural identity by dominant groups, while social trauma encompasses long-term societal abuses that threaten a community's sense of belonging.
These traumas contribute to a pervasive mistrust in healthcare systems, as evidenced by past abuses such as the Tuskegee Syphilis Experiment and unethical medical practices targeting minority groups. Understanding these traumas is crucial for practitioners aiming to build trust with patients from these communities.
Implementing Trauma-Informed Care
Practitioners can improve their skills by adopting a trauma-informed approach to care. This involves recognizing the signs of trauma and integrating knowledge about its effects into all aspects of service delivery. Key strategies include:
- Cultural Sensitivity: Tailor interventions to respect and incorporate cultural values and practices. This helps bridge the gap between healthcare providers and patients from diverse backgrounds.
- Community Engagement: Work collaboratively with community leaders to develop interventions that address specific needs and concerns. Community-based participatory research (CBPR) is an effective method for achieving this.
- Building Trust: Establish transparent communication channels and provide consistent, reliable information about healthcare services. This helps dismantle barriers created by historical mistrust.
The Role of Practitioners in Healing
The study suggests that transformative interventions are necessary to address the fear and mistrust present in these communities. Practitioners can play a vital role by facilitating restorative circles—safe spaces where community members can share their experiences without fear of judgment. These circles promote healing by fostering a sense of belonging and trust within the community.
Moreover, practitioners should advocate for policies that address social determinants of health, such as income inequality and access to education. By tackling these root causes, healthcare providers can contribute to long-term improvements in health outcomes for marginalized populations.
Encouraging Further Research
The findings from this study underscore the need for ongoing research into culturally sensitive public health interventions. Practitioners are encouraged to collaborate with academic institutions and community organizations to explore new models of care that prioritize the unique needs of communities of color.
By participating in or initiating research projects, practitioners can help develop evidence-based strategies that reduce health disparities and promote equity in healthcare access.
Conclusion
The "Continuum of Trauma" model provides a valuable framework for understanding how historical, cultural, and social traumas influence healthcare decision-making among communities of color. By adopting trauma-informed care practices and engaging with communities through culturally sensitive approaches, practitioners can help rebuild trust in healthcare institutions.