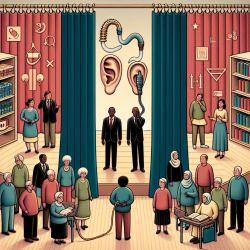
As a practitioner committed to creating great outcomes for children, it is essential to stay informed about the factors that influence the effectiveness of treatments like cochlear implants (CIs). The research article "Defining Disparities in Cochlear Implantation through the Social Determinants of Health" offers valuable insights into the disparities that exist in CI access and outcomes, shaped by various social determinants of health (SDH).
The social determinants of health framework encompasses five domains: healthcare access/quality, education access/quality, social and community context, economic stability, and neighborhood/physical environment. Understanding these domains can help practitioners identify and address the barriers faced by their patients, leading to more equitable and effective care.
Healthcare Access and Quality
Access to quality healthcare is critical for optimal CI outcomes. Factors such as geographic location, insurance coverage, and availability of specialized providers can significantly impact a patient's ability to receive timely and effective CI care. Practitioners should consider these factors when developing care plans and advocate for policies that improve healthcare access for underserved populations.
Education Access and Quality
Educational attainment and health literacy are closely linked to health outcomes. Parents' educational levels can influence their children's utilization of hearing healthcare and speech development post-CI. Practitioners can support families by providing resources and education to improve health literacy and encourage early intervention.
Social and Community Context
Social support systems play a vital role in the success of CI treatment. Children and adults with strong social networks are more likely to adhere to their treatment plans and experience better outcomes. Practitioners should involve family members and community resources in the care process to enhance social support for their patients.
Economic Stability
Economic factors such as income, employment, and housing security can affect a patient's ability to access and adhere to CI treatment. Practitioners should be aware of these challenges and work to connect families with financial assistance programs and other resources to support their treatment journey.
Neighborhood and Physical Environment
The quality of a patient's living environment can impact their overall health and access to healthcare services. Practitioners should consider environmental factors such as housing conditions and transportation availability when developing care plans and advocate for improvements in community infrastructure to support better health outcomes.
To further enhance your understanding and application of these concepts, consider utilizing validated assessment tools like the Health-Related Social Needs Screening Tool or the PRAPARE tool to systematically evaluate SDH factors in your patients. Incorporating this information into your practice can help you develop targeted interventions that address disparities and promote health equity.
For a more in-depth exploration of these topics, I encourage you to read the original research paper, Defining Disparities in Cochlear Implantation through the Social Determinants of Health.