Introduction
As speech-language pathologists, we are committed to improving the lives of our patients through evidence-based practices. One area of growing concern is postextubation dysphagia, a condition that affects many survivors of critical illness who required mechanical ventilation. The research article "Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness" by Macht et al. provides valuable insights into the prevalence, risk factors, and outcomes associated with this condition. This blog aims to help practitioners enhance their skills by implementing the findings of this research or encouraging further study.
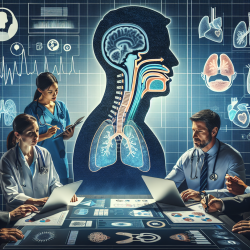
Understanding Postextubation Dysphagia
Postextubation dysphagia refers to swallowing difficulties that arise after the removal of an endotracheal tube. According to Macht et al., this condition is common among survivors of critical illness, with an incidence rate of 84% among patients who underwent a bedside swallow evaluation (BSE). The study found that long durations of mechanical ventilation and reintubation were significant risk factors for severe dysphagia. Furthermore, the presence of severe dysphagia was independently associated with poor patient outcomes, including pneumonia, reintubation, in-hospital mortality, and prolonged hospital stays.
Key Findings and Their Implications
The study by Macht et al. provides several key findings that can guide clinical practice:
- High Prevalence: Postextubation dysphagia was present in 84% of patients who underwent BSE, indicating a high prevalence among survivors of mechanical ventilation.
- Risk Factors: Long durations of mechanical ventilation (more than seven days) and reintubation were significant risk factors for developing severe dysphagia.
- Poor Outcomes: Severe dysphagia was associated with increased risks of pneumonia, reintubation, in-hospital mortality, and prolonged hospital stays.
Implementing Research Findings in Clinical Practice
To improve patient outcomes, practitioners can implement the following strategies based on the research findings:
Early Identification and Assessment
Given the high prevalence of postextubation dysphagia, early identification and assessment are crucial. Practitioners should prioritize conducting bedside swallow evaluations (BSE) for patients who have undergone mechanical ventilation, especially those with prolonged intubation durations.
Risk Factor Management
Understanding the risk factors for severe dysphagia can help practitioners develop targeted interventions. For instance, minimizing the duration of mechanical ventilation and avoiding reintubation whenever possible can reduce the risk of severe dysphagia.
Multidisciplinary Approach
Managing postextubation dysphagia requires a multidisciplinary approach involving speech-language pathologists, respiratory therapists, and critical care physicians. Collaborative care can ensure comprehensive assessment and intervention strategies tailored to each patient's needs.
Ongoing Monitoring and Follow-Up
Postextubation dysphagia often persists at the time of discharge. Therefore, ongoing monitoring and follow-up are essential to address any lingering swallowing difficulties and prevent complications such as pneumonia and malnutrition.
Encouraging Further Research
While the study by Macht et al. provides valuable insights, further research is needed to explore the underlying mechanisms of postextubation dysphagia and develop effective diagnostic and treatment strategies. Practitioners are encouraged to contribute to this growing body of knowledge by conducting research and sharing their findings with the broader medical community.
Conclusion
Postextubation dysphagia is a prevalent and serious condition among survivors of critical illness. By implementing the findings of the research by Macht et al., practitioners can enhance their skills and improve patient outcomes. Early identification, risk factor management, a multidisciplinary approach, and ongoing monitoring are key strategies to address this condition effectively.
To read the original research paper, please follow this link: Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness.