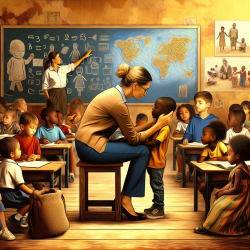
The role of Traditional Birth Attendants (TBAs) in maternal healthcare has been a topic of debate for decades. In many low-resource settings, TBAs have been the cornerstone of childbirth assistance. However, their integration into formal healthcare systems has often been limited. The research article "Training Traditional Birth Attendants on the Use of Misoprostol and a Blood Measurement Tool to Prevent Postpartum Haemorrhage: Lessons Learnt from Bangladesh" sheds light on how targeted training can significantly impact maternal health outcomes.
The Importance of Training TBAs
The study conducted in Bangladesh between July 2009 and July 2010 involved training TBAs to use misoprostol and a blood measurement tool to prevent postpartum hemorrhage (PPH) during home deliveries. This initiative was driven by the need to address PPH, a leading cause of maternal mortality worldwide.
The training focused on equipping TBAs with knowledge about the administration of misoprostol—a drug that helps prevent excessive bleeding after childbirth—and the use of an absorbent mat to measure blood loss accurately. These tools are crucial in settings where access to skilled birth attendants is limited.
Key Outcomes and Impacts
- Direct Intervention Impacts: The use of misoprostol and the blood measurement tool led to safer home deliveries with reduced instances of excessive bleeding. TBAs reported a decrease in the need for emergency referrals due to improved management of PPH.
- Strengthened Healthcare Linkages: The training fostered stronger connections between TBAs and formal healthcare providers. This collaboration improved referral systems and enhanced respect for TBAs within the healthcare community.
- Community Trust and Communication: TBAs gained increased trust from their communities, leading to more open communication and higher acceptance of maternal health interventions. This trust was pivotal in encouraging more women to seek antenatal care (ANC).
- Improved Service Utilization: The perceived quality of care improved, with more women registering for ANC services. This increase was attributed to the community's growing awareness of the benefits of using misoprostol and the mat during delivery.
Lessons for Practitioners
The findings from this study offer valuable insights for practitioners aiming to enhance maternal health outcomes in similar settings:
- Embrace Training and Education: Continuous education and training for TBAs can lead to significant improvements in maternal health outcomes. Practitioners should advocate for regular training sessions that focus on lifesaving interventions like misoprostol.
- Cultivate Community Relationships: Building trust within communities is essential. Practitioners should engage with local leaders and families to promote understanding and acceptance of new health practices.
- Create Strong Referral Systems: Establishing robust referral pathways between TBAs and formal healthcare facilities ensures timely interventions during emergencies, reducing maternal mortality risks.
- Pursue Further Research: While this study highlights positive changes, further research is needed to quantify these impacts across different regions. Practitioners should support studies that explore the scalability of such interventions.
A Call to Action
This study underscores the transformative potential of integrating TBAs into formal healthcare systems through targeted training programs. By equipping them with essential tools like misoprostol and blood measurement devices, we can significantly reduce maternal mortality rates associated with PPH.
If you are a practitioner looking to make a difference in maternal health care, consider implementing similar training programs in your area. Encourage collaboration between TBAs and healthcare professionals to create a cohesive network that supports safer childbirth practices.