Introduction
The journey of pregnancy and postpartum is a transformative experience, yet it can be accompanied by significant challenges, particularly concerning pain management. The recent study, "Trajectories of Pain Intensity, Pain Catastrophizing, and Pain Interference in the Perinatal and Postpartum Period," provides valuable insights into understanding and addressing these challenges. This blog aims to guide practitioners in leveraging these findings to enhance maternal care and outcomes.
Understanding Pain Trajectories
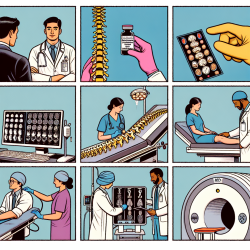
The study identifies distinct trajectories of pain intensity, pain catastrophizing, and pain interference during pregnancy and postpartum. The data reveals that while pain intensity remains relatively homogeneous, pain catastrophizing and interference exhibit significant variability. These findings emphasize the importance of recognizing individual pain experiences and tailoring interventions accordingly.
Implications for Practitioners
For practitioners, understanding these trajectories is crucial in identifying women at high risk for adverse pain outcomes. The study highlights the association between baseline symptoms of anxiety, depression, insomnia, and pain symptomology with pain trajectories. By assessing these factors early, practitioners can develop targeted management strategies to prevent chronic pain development during pregnancy and postpartum.
Data-Driven Interventions
Implementing data-driven interventions can significantly improve maternal care. Practitioners are encouraged to:
- Regularly assess pain intensity, catastrophizing, and interference throughout pregnancy and postpartum.
- Monitor mental health indicators such as anxiety, depression, and insomnia, which are linked to pain trajectories.
- Develop personalized pain management plans, considering individual risk factors and pain experiences.
Encouraging Further Research
While this study provides a robust foundation, further research is essential to deepen our understanding of pain trajectories and their implications. Practitioners are encouraged to contribute to ongoing research efforts, exploring diverse populations and integrating new methodologies to enhance maternal care.
Conclusion
By embracing data-driven insights and personalized interventions, practitioners can significantly impact maternal health outcomes. The findings from this study serve as a call to action, urging practitioners to integrate these insights into their practice and contribute to a future where every woman receives the care she deserves.
To read the original research paper, please follow this link: Trajectories of pain intensity, pain catastrophizing, and pain interference in the perinatal and postpartum period.