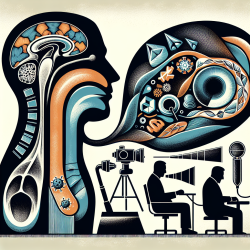
Dysphagia, characterized by difficulty in swallowing, is a prevalent condition among the elderly. With an aging population, the need for accurate diagnosis and effective management of dysphagia has become increasingly important. The research article "The Role of Imaging Modalities in Diagnosing Dysphagia: A Clinical Review" provides a comprehensive overview of various imaging techniques that can aid practitioners in diagnosing and managing this condition more effectively.
Understanding Dysphagia in the Elderly
Dysphagia is broadly classified into oropharyngeal and esophageal types. Oropharyngeal dysphagia involves difficulty in moving food from the mouth to the esophagus, while esophageal dysphagia pertains to issues within the esophagus itself. The elderly are particularly susceptible to dysphagia due to age-related changes and comorbid conditions.
Key Imaging Modalities
- Fiberoptic Endoscopic Evaluation of Swallowing (FEES): This bedside procedure involves passing a flexible endoscope through the nose to assess swallowing safety and efficacy. It is particularly useful for patients who cannot be easily transported or positioned for other tests.
- Videofluoroscopic Swallow Study (VFSS): Often considered the gold standard, VFSS uses fluoroscopy to provide real-time imaging of the swallowing process. It helps identify aspiration risks and underlying causes of dysphagia.
- High-Resolution Pharyngeal Manometry (HRPM): An emerging technique that measures pharyngeal pressure during swallowing, HRPM offers detailed insights into pharyngeal muscle function and is valuable for patients with neurological disorders.
- Barium Swallow: This non-invasive test evaluates esophageal motility and structure but does not allow for therapeutic interventions like biopsies.
- Esophagogastroduodenoscopy (EGD): Preferred for suspected esophageal dysphagia, EGD allows direct visualization and biopsy of the esophagus but is invasive and requires sedation.
- High-Resolution Esophageal Manometry (HREM): Adds depth to diagnosing esophageal motility disorders by providing detailed pressure topography.
Implementing Research Outcomes in Practice
The review article emphasizes that each imaging modality has unique advantages and limitations. Practitioners should consider factors such as patient condition, suspected etiology, and available resources when selecting an appropriate diagnostic tool. By integrating these imaging techniques into clinical practice, healthcare providers can improve diagnostic accuracy and tailor treatment strategies effectively.
Encouraging Further Research
The evolving landscape of dysphagia diagnosis calls for continuous research and adaptation. Practitioners are encouraged to stay informed about advancements in imaging technologies and their applications in clinical settings. By doing so, they can enhance their diagnostic acumen and contribute to better patient outcomes.
To read the original research paper, please follow this link: The Role of Imaging Modalities in Diagnosing Dysphagia: A Clinical Review.