Introduction
The involvement of service users and caregivers is a pivotal strategy in strengthening mental health systems, particularly in low-and-middle-income countries (LMICs). This blog explores the application of a Theory of Change (ToC) model to enhance service user and caregiver involvement in rural Ethiopia's primary healthcare system. The research conducted by Abayneh et al. (2020) provides a comprehensive framework for understanding and implementing these complex interventions.
Understanding the Theory of Change Model
The ToC model is a participatory approach that outlines the processes and pathways necessary for achieving long-term outcomes in mental health system strengthening. It involves stakeholders at various levels, including community members, health organizations, service users, and caregivers, to collaboratively develop and refine strategies for effective involvement.
Key Components of the ToC Model
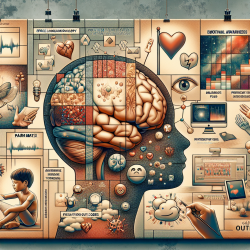
The ToC model developed in Ethiopia incorporates several key components:
- Community Engagement: Mobilizing resources and raising awareness about mental health to support service users and caregivers.
- Health Organization Support: Ensuring the availability of mental health services and competent care providers within primary healthcare settings.
- Service User Empowerment: Establishing service user groups to advocate for mental health services and provide peer support.
- Caregiver Involvement: Collaborating with service user groups to enhance advocacy and support for mental health services.
Implementing the ToC Model
For practitioners looking to implement the ToC model, it is essential to engage stakeholders at all levels actively. This involves conducting workshops and consultative meetings to refine strategies and ensure all voices are heard. Capacity-building training for community leaders, health professionals, and service users is crucial to equip them with the necessary skills and knowledge for effective involvement.
Challenges and Opportunities
While the ToC model offers a robust framework for service user and caregiver involvement, challenges such as stigma, resource limitations, and logistical barriers must be addressed. However, the participatory nature of the ToC process fosters collaboration and commitment among stakeholders, creating opportunities for sustainable change and improved mental health outcomes.
Conclusion
The ToC model provides a valuable tool for practitioners seeking to enhance mental health systems in rural Ethiopia and similar settings. By involving service users and caregivers in the decision-making process, mental health services can become more accessible, acceptable, and effective.
To read the original research paper, please follow this link: Developing a Theory of Change model of service user and caregiver involvement in mental health system strengthening in primary health care in rural Ethiopia.