Introduction
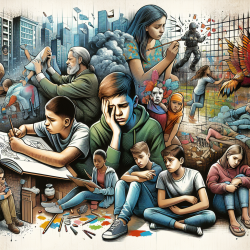
In the evolving landscape of pediatric healthcare, addressing obesity in children and adolescents is paramount. The recent Obesity Pillars roundtable: Metabolic and bariatric surgery in children and adolescents provides crucial insights into the role of metabolic and bariatric surgery (MBS) in managing severe obesity in young patients. This blog explores how practitioners can leverage these findings to improve outcomes for children and adolescents struggling with obesity.
Understanding the Research
The roundtable discussion brings together experts who highlight the necessity of MBS as part of a comprehensive treatment plan for pediatric obesity. The study emphasizes that children and adolescents with severe obesity, defined as a BMI ≥120% of the 95th percentile, should be considered for MBS, especially when obesity-related complications are present.
Key Findings and Implications
- Early Intervention: The research underscores the importance of early intervention in preventing long-term complications associated with obesity, such as cardiovascular diseases and type 2 diabetes.
- Comprehensive Care: MBS should be integrated with medication, nutrition, behavioral training, and physical activity to ensure holistic care.
- Inclusion Criteria: Children with cognitive disabilities or mental health issues should not be excluded from MBS if their conditions are well-managed.
- Family Involvement: Successful outcomes often depend on the involvement of family members, highlighting the need for family-based therapy.
Practical Applications for Practitioners
Practitioners can enhance their clinical practice by incorporating the following strategies based on the research findings:
- Early Screening and Referral: Implement routine screening for obesity-related complications and consider early referral for MBS when appropriate.
- Multidisciplinary Approach: Collaborate with dietitians, psychologists, and pediatricians to create a comprehensive care plan tailored to each child's needs.
- Family-Centered Care: Engage families in the treatment process to ensure they provide the necessary support and environment for the child's success.
- Ongoing Education: Stay informed about the latest guidelines and research to provide evidence-based care.
Encouraging Further Research
While the current research provides valuable insights, ongoing studies are essential to refine treatment protocols and improve outcomes. Practitioners are encouraged to participate in research initiatives and contribute to the growing body of knowledge on pediatric obesity and MBS.
Conclusion
The integration of MBS into pediatric obesity treatment represents a significant advancement in addressing this chronic condition. By adopting a data-driven, comprehensive approach, practitioners can significantly improve the quality of life for children and adolescents affected by severe obesity.
To read the original research paper, please follow this link: Obesity Pillars roundtable: Metabolic and bariatric surgery in children and adolescents.