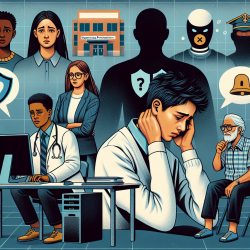
Stigma and discrimination related to mental health and substance use issues are significant barriers in primary health care (PHC) settings. A recent qualitative study conducted in Toronto, Canada, sheds light on the experiences of health providers and their clients in Community Health Centres (CHCs). This research highlights the complex interplay of stigma, discrimination, and the social determinants of health that affect marginalized populations. As practitioners, understanding these dynamics is crucial for improving care delivery and client outcomes.
The Impact of Stigma and Discrimination
The study reveals that PHC settings often become sites where clients face multiple forms of stigma. These stigmas are not only related to mental health and substance use (MHSU) issues but also intersect with factors such as gender, race, class, age, and visibility of distress. This intersectionality creates barriers to accessing care and can exacerbate the challenges faced by clients.
Health providers in CHCs encounter a diverse clientele, including Indigenous people, immigrants, refugees, street-involved youth, and transgender individuals. These groups often experience compounded stigmas due to socio-cultural beliefs and systemic discrimination. For instance, cultural misunderstandings between clients and providers can lead to alienation and hinder effective communication.
Strategies for Practitioners
To address these challenges, practitioners can implement several strategies based on the study's findings:
- Training and Education: Continuous training on anti-stigma practices is essential. Providers should engage in regular sessions that integrate into daily practice rather than one-off workshops. Tailored training for different roles within CHCs can enhance understanding and empathy.
- Communication Skills: Developing excellent listening skills is crucial for understanding clients' needs. Practitioners should be mindful of language use to avoid perpetuating stigma. For example, avoiding terms like "clean" when referring to someone who is not using drugs can help reduce negative connotations.
- Community Engagement: Anti-stigma campaigns within local communities can mitigate negative interactions outside CHCs. Collaborating with local businesses, social service agencies, and residents can foster a supportive environment for clients.
- Recovery-Oriented Approaches: Emphasizing recovery as a dynamic process rather than an end-state can empower clients. Practitioners should focus on harm reduction and support clients in finding meaning despite MHSU challenges.
The Role of Community Health Centres
CHCs play a pivotal role in addressing stigma by integrating services that consider the social determinants of health. These centres offer interdisciplinary care that includes community outreach workers and peer support staff. By focusing on community development and eliminating systemic barriers such as poverty and racism, CHCs are better equipped to serve marginalized populations effectively.
Encouraging Further Research
The study underscores the need for ongoing research into effective anti-stigma interventions within PHC settings. Practitioners are encouraged to explore innovative approaches that address local needs and specific behaviors of well-defined groups. By participating in research initiatives or collaborating with academic institutions, practitioners can contribute to developing evidence-based strategies that improve health outcomes for marginalized communities.
To read the original research paper, please follow this link: Stigma and discrimination related to mental health and substance use issues in primary health care in Toronto, Canada: a qualitative study.