Interstitial cystitis/bladder pain syndrome (IC/BPS) is a chronic condition that significantly impacts the lives of those affected. A recent qualitative study by McKernan et al. sheds light on the treatment needs of individuals with IC/BPS, emphasizing the importance of patient-centered interventions. This blog explores how practitioners can enhance their skills by implementing insights from this research.
The Complex Nature of IC/BPS
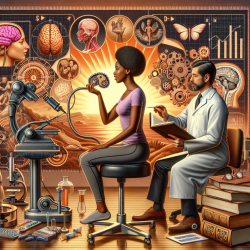
IC/BPS is characterized by pelvic pain, urinary urgency and frequency, and bladder pressure. The condition often coexists with psychosocial comorbidities such as anxiety, depression, and trauma-related symptoms, which exacerbate the illness. Despite the prevalence of these psychological challenges, there is a notable lack of interdisciplinary mental health intervention in urology.
Key Findings from the Research
The study utilized focus groups and self-report assessments to gather data from 27 female participants with IC/BPS. Five major themes emerged:
- Managing Physical Symptoms: Participants reported challenges with bladder and pelvic pain, sleep difficulties, nausea, and fatigue.
- Emotional Symptoms: Emotional distress was both a precursor and a consequence of physical symptoms, highlighting a cyclical relationship between stress and symptom severity.
- Impact on Daily Life: IC/BPS affected participants' social interactions, romantic relationships, and ability to work or travel.
- Response to Illness: Coping strategies varied from adaptive (seeking support) to maladaptive (social withdrawal).
- Addressing Needs in Treatment: Participants expressed a need for better education on IC/BPS and integrated psychological care.
Implications for Practitioners
The findings suggest several ways practitioners can improve their approach to managing IC/BPS:
- Tailored Psychological Interventions: Focus on pain management, emotion regulation, communication skills, and addressing sexual dysfunction.
- Interdisciplinary Collaboration: Work closely with mental health professionals to provide comprehensive care that addresses both physiological and psychological aspects of IC/BPS.
- Patient Education: Develop reliable educational materials to empower patients with knowledge about their condition and treatment options.
- Cognitive-Behavioral Approaches: Implement cognitive-behavioral strategies that are specific to IC/BPS to enhance patient coping mechanisms and improve quality of life.
The Path Forward: Encouraging Further Research
This study highlights the need for further research into effective psychological interventions for IC/BPS. Practitioners are encouraged to contribute to this growing body of knowledge by exploring innovative treatment approaches and sharing their findings with the medical community.