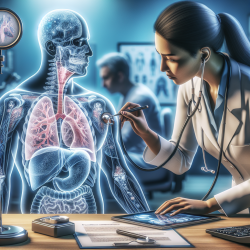
Chronic Obstructive Pulmonary Disease (COPD) is a prevalent condition that significantly impacts patients' quality of life. One often overlooked aspect of COPD is its association with swallowing impairments or dysphagia. Recent research published in the International Journal of Chronic Obstructive Pulmonary Disease sheds light on the complexities of oropharyngeal swallow physiology in underweight patients with advanced COPD. This blog explores key findings from the study and offers insights for practitioners looking to enhance their skills and improve patient outcomes.
The Study Overview
The study conducted by Garand et al. focused on ten underweight patients with stable but advanced-stage COPD. These patients underwent a modified barium swallow study to assess their swallowing function using standardized metrics such as the Modified Barium Swallow Impairment Profile (MBSImP) and the Penetration–Aspiration Scale (PAS). The results were compared with those of age- and sex-matched healthy controls.
Key Findings
- Oral Impairment: COPD patients exhibited significantly higher MBSImP oral total scores compared to controls, indicating notable oral impairment.
- Airway Invasion: The maximum PAS scores were significantly higher in COPD patients, suggesting an increased risk of airway invasion during swallowing.
- Patient Perception: Despite these impairments, there was no significant difference in patient-reported swallowing difficulties between COPD patients and controls.
Implications for Practitioners
The study highlights the need for practitioners to be vigilant about potential swallowing impairments in COPD patients, especially those who are underweight. Here are some ways practitioners can apply these findings:
- Comprehensive Assessment: Incorporate thorough swallowing assessments into routine evaluations for COPD patients. Utilize tools like MBSImP to identify specific impairments.
- Patient Education: Educate patients about the risks associated with dysphagia and encourage them to report any difficulties they experience during eating or drinking.
- Nutritional Support: Collaborate with dietitians to ensure that underweight patients receive adequate nutritional support to mitigate the effects of dysphagia.
- Interdisciplinary Approach: Work closely with speech-language pathologists and other healthcare professionals to develop comprehensive management plans tailored to individual patient needs.
The Need for Further Research
The study underscores the complexity of swallowing impairments in COPD and suggests areas for further research. Future studies should explore the interaction between respiratory-swallowing systems and investigate potential interventions that could improve swallowing function in this population.
Conclusion
The findings from this study provide valuable insights into the challenges faced by underweight COPD patients with dysphagia. By incorporating these insights into practice, healthcare professionals can enhance their skills and improve patient outcomes. Continuous research and interdisciplinary collaboration are essential to developing effective strategies for managing dysphagia in COPD patients.
To read the original research paper, please follow this link: Oropharyngeal swallow physiology and swallowing-related quality of life in underweight patients with concomitant advanced chronic obstructive pulmonary disease.