The role of accompanying patients (APs) in clinical oncology teams has been gaining attention for its potential to improve patient care and practitioner skills. The research article "Accompanying patients in clinical oncology teams: Reported activities and perceived effects" provides valuable insights into how APs can enhance the experience of cancer patients and support healthcare professionals. This blog explores how practitioners can implement these findings to improve their skills and encourages further research in this area.
The Role of Accompanying Patients (APs)
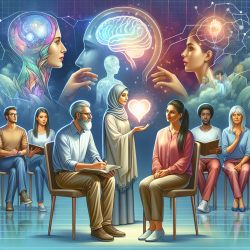
APs are individuals who have undergone cancer treatment themselves and now serve as patient advisors within clinical teams. Their primary role is to provide emotional, informational, and educational support to current patients undergoing treatments such as radiotherapy, chemotherapy, or surgery. By sharing their personal experiences, APs help patients feel understood and supported, alleviating stress and empowering them to become active participants in their care.
Key Activities of APs
- Emotional Support: APs offer empathetic listening and validate patients' emotions, helping them navigate the complexities of their cancer journey.
- Navigational Support: They guide patients through the healthcare system, ensuring they are aware of available resources and their rights.
- Informational Support: APs share personal experiences to help patients understand medical information and prepare for appointments.
- Collaboration with Clinical Teams: By acting as a liaison between patients and healthcare professionals, APs enhance communication and streamline patient care processes.
The Impact on Practitioners
The integration of APs into oncology teams not only benefits patients but also provides opportunities for practitioners to enhance their skills. Here are some ways practitioners can leverage the presence of APs:
- Improved Communication: By observing APs' interactions with patients, practitioners can learn effective communication techniques that foster trust and openness.
- Cultural Competence: Understanding the diverse experiences of APs can help practitioners develop cultural competence, enabling them to provide more personalized care.
- Emotional Intelligence: Engaging with APs can enhance practitioners' emotional intelligence, allowing them to better empathize with patients' experiences.
The Benefits of Peer Support
The research highlights several benefits of peer support in oncology settings. Patients who engage with APs often report feeling less anxious and more prepared for medical appointments. This reduction in stress can lead to better adherence to treatment plans and improved health outcomes. Additionally, the presence of APs can alleviate some of the workload on clinical teams by providing complementary emotional support.
Encouraging Further Research
The concept of integrating APs into clinical teams is relatively new, and there is much to learn about its long-term effects on both patients and healthcare providers. Practitioners are encouraged to conduct further research on this topic to explore different models of integration and assess the impact on various healthcare settings.
The research article "Accompanying patients in clinical oncology teams: Reported activities and perceived effects" serves as a valuable resource for those interested in this field. To read the original research paper, please follow this link: Accompanying patients in clinical oncology teams: Reported activities and perceived effects.