Understanding NMDAR Dysfunction in Schizophrenia
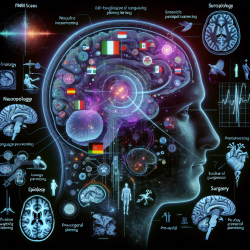
The recent research article, "Functional connectivity signatures of NMDAR dysfunction in schizophrenia—integrating findings from imaging genetics and pharmaco-fMRI," offers profound insights into the pathophysiology of schizophrenia. The study explores how N-methyl-D-aspartate receptor (NMDAR) dysfunction contributes to schizophrenia, suggesting a major role in the disease's excitatory/inhibitory (E/I) imbalance.
Key Findings and Implications
By integrating imaging genetics and pharmaco-fMRI data, the study identifies shared functional connectivity signatures associated with genetically and pharmacologically induced NMDAR dysfunction. These findings could pave the way for developing biomarkers to stratify patients based on common molecular pathways, thus enabling personalized treatment approaches.
- Genetic Insights: The study highlights the GRIN2A genetic variant's role in schizophrenia, associated with language-related negative symptomatology and altered functional connectivity.
- Pharmacological Comparisons: The research compares the effects of the NMDAR antagonist ketamine and the GABA-A receptor agonist midazolam, revealing their contrasting impacts on neural connectivity.
- Functional Connectivity Patterns: Increased connectivity between striato-pallido-thalamic regions and cortical areas, and decreased connectivity between auditory and visual processing regions were observed, indicating an E/I imbalance.
Practical Applications for Practitioners
Practitioners can leverage these findings to enhance their therapeutic strategies:
- Patient Stratification: Utilize identified biomarkers for patient stratification to tailor interventions based on individual genetic profiles.
- Targeted Therapies: Focus on therapies that address the E/I imbalance, potentially using pharmacological agents that modulate NMDAR activity.
- Further Research: Encourage further research into the functional connectivity profiles of patients, which may reveal additional therapeutic targets.
Encouraging Further Exploration
While the study provides a robust framework for understanding NMDAR dysfunction in schizophrenia, it also opens avenues for further research. Practitioners are encouraged to explore additional genetic variants and their impacts on neural connectivity and symptomatology. Moreover, investigating other pharmacological agents' effects on NMDAR activity could yield new therapeutic options.
Conclusion
The integration of genetic and pharmacological data in understanding NMDAR dysfunction in schizophrenia marks a significant step toward personalized psychiatry. By identifying shared functional connectivity signatures, this research not only enhances our understanding of schizophrenia's pathophysiology but also lays the groundwork for more effective, individualized treatments.
To read the original research paper, please follow this link: Functional connectivity signatures of NMDAR dysfunction in schizophrenia—integrating findings from imaging genetics and pharmaco-fMRI.