Introduction
Down Syndrome (DS) is a genetic disorder characterized by intellectual disability and a range of physical and cognitive abnormalities. Recent research, such as the study by McCann et al. (2021), has utilized structural magnetic resonance imaging (MRI) to identify volumetric brain abnormalities in individuals with DS, spanning from newborns to young adults. These findings have significant implications for speech-language pathologists (SLPs) who work with children with DS. By understanding these brain abnormalities, practitioners can tailor their therapeutic approaches to better address the unique needs of this population.
Key Findings from the Study
The study identified several key volumetric abnormalities in the brains of individuals with DS:
- Increased volumes in the perirhinal and entorhinal cortices, which are crucial for memory processing.
- Increased volumes in Brodmann’s areas (BA) 3a, 3b, and 44, which are involved in sensory and motor functions, as well as speech production.
- Decreased volumes in the white matter of the cuneus, paracentral lobule, postcentral gyrus, and supramarginal gyrus, which are associated with sensory and motor deficits.
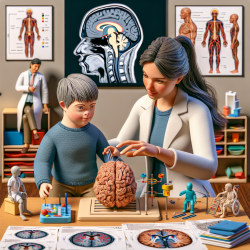
Implications for Speech and Language Therapy
Understanding these brain abnormalities can help SLPs develop more effective, data-driven therapeutic interventions. Here are some ways to implement these findings:
1. Focus on Memory-Related Interventions
Given the increased volumes in the perirhinal and entorhinal cortices, which are involved in memory, SLPs should incorporate memory-enhancing activities into their therapy sessions. Techniques such as spaced repetition, mnemonic devices, and visual aids can be particularly beneficial.
2. Address Speech Production Deficits
The increased volume in BA 44, part of Broca’s area, highlights the importance of targeting speech production. SLPs can use techniques like phonemic drills, articulation exercises, and speech modeling to improve expressive language skills.
3. Sensory Integration Therapy
The decreased volumes in the white matter of sensory-related brain regions suggest that children with DS may benefit from sensory integration therapy. Activities that stimulate proprioception, tactile, and vestibular senses can help improve motor coordination and sensory processing.
4. Multimodal Approaches
Given the complex nature of brain abnormalities in DS, a multimodal approach that combines various therapeutic techniques can be more effective. This includes integrating speech therapy with occupational and physical therapy to address both cognitive and motor deficits comprehensively.
Encouraging Further Research
While the study by McCann et al. provides valuable insights, further research is needed to explore the long-term effects of these brain abnormalities and their impact on therapy outcomes. Practitioners are encouraged to stay updated with the latest research and consider participating in studies that aim to develop and validate new therapeutic approaches.
Conclusion
By leveraging the findings from structural MRI studies, SLPs can make data-driven decisions to enhance their therapeutic interventions for children with DS. Understanding the specific brain abnormalities allows for more targeted and effective therapy, ultimately leading to better outcomes for children.
To read the original research paper, please follow this link: Structural magnetic resonance imaging demonstrates volumetric brain abnormalities in down syndrome: Newborns to young adults.