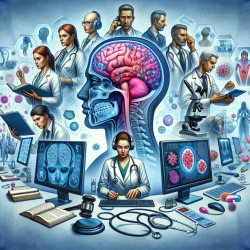
The recent research article titled "The importance of basal-temporal white matter to pre- and post-surgical naming ability in temporal lobe epilepsy" sheds light on a critical aspect of cognitive function in patients with temporal lobe epilepsy (TLE). This study highlights the significance of white matter integrity in the basal-temporal region, particularly its impact on naming abilities both before and after surgical intervention.
The Study's Core Findings
The research underscores that healthier basal-temporal white matter is linked to better naming abilities. Specifically, the study found that higher fractional anisotropy (FA) in certain white matter tracts correlates with improved visual and auditory naming scores. These findings are crucial for practitioners working with TLE patients, as they provide a deeper understanding of the structural underpinnings that support language functions.
Pre-Surgical Implications
Before surgery, patients with higher FA in bilateral inferior longitudinal fasciculus (ILF), inferior frontal occipital fasciculus (IFOF), and left fusiform superficial white matter (SWM) exhibited superior naming performance. This suggests that maintaining the integrity of these tracts could be pivotal in preserving cognitive functions related to language.
Post-Surgical Outcomes
The study also reveals that post-surgical naming decline is less pronounced in patients with healthier right hemisphere fusiform-associated white matter. This finding is particularly relevant for practitioners aiming to mitigate cognitive decline following anterior temporal lobectomy (ATL).
Practical Applications for Practitioners
For practitioners, these insights can be transformative. By focusing on preserving or enhancing the integrity of specific white matter tracts, therapists can potentially improve language outcomes for TLE patients. Here are some practical steps:
- Pre-Surgical Assessment: Incorporate advanced imaging techniques like diffusion-weighted MRI to assess white matter integrity. This can help identify patients at risk for post-surgical cognitive decline.
- Tailored Therapy Plans: Develop individualized therapy plans that focus on strengthening language networks. This could involve targeted cognitive exercises designed to enhance lexical-semantic processing.
- Post-Surgical Monitoring: Regularly monitor language abilities post-surgery to identify any decline early. This allows for timely intervention and adjustment of therapeutic strategies.
Encouraging Further Research
This study opens avenues for further research into the relationship between white matter integrity and language functions. Practitioners are encouraged to engage in collaborative studies that explore innovative therapeutic approaches based on these findings. Such efforts could lead to more effective interventions and improved quality of life for TLE patients.
Conclusion
The insights from this research emphasize the importance of basal-temporal white matter in supporting naming abilities in TLE patients. By integrating these findings into clinical practice, practitioners can enhance their therapeutic strategies and contribute to better patient outcomes.
To read the original research paper, please follow this link: The importance of basal-temporal white matter to pre- and post-surgical naming ability in temporal lobe epilepsy.