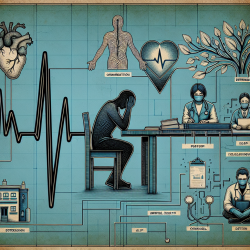
The COVID-19 pandemic has left a significant mark on various aspects of life, with youth mental health being one of the most affected areas. The abrupt transition from in-person to remote learning and the closure of school-based health centers (SBHCs) disrupted access to essential mental health services for many students. This blog post delves into the findings from the research article "The Impact of School Closures on Service Utilization in School-Based Health Centers" and explores how practitioners can enhance their skills by implementing these findings or pursuing further research.
The Impact of School Closures on Mental Health Services
The pandemic-induced school closures led to a substantial decline in mental health service utilization despite an increase in mental health needs among students. The study analyzed data from three large public high schools and found a 34% decline in the average number of patients seen for behavioral health services between 2018-2019 and 2020-2021. This decline was particularly pronounced during the transition to telehealth services.
The shift to telehealth compromised many advantages associated with SBHCs, such as convenience, easy access, and face-to-face support. The lack of direct walk-in access and reduced teacher-student interactions contributed to decreased referrals for mental health treatment. Moreover, students' motivation to seek help diminished due to isolation and deteriorating mental health.
Telehealth vs. In-Person Care: A Comparative Analysis
The study highlighted that telehealth services alone were less effective than in-person or hybrid models in maintaining service utilization levels. An analysis revealed a 60% decrease in patients seen for behavioral health treatment when shifting from in-person care to telehealth. Even after schools reopened for in-person learning, service utilization did not return to pre-pandemic levels until SBHCs offered hybrid care.
This finding underscores the importance of maintaining some level of in-person interaction for initial evaluations while leveraging telehealth's flexibility for ongoing treatment. Practitioners should consider optimizing combinations of service modalities based on individual student needs.
Recommendations for Practitioners
- Enhance Awareness: Educators and practitioners should be vigilant about students' mental well-being and encourage open communication to facilitate timely referrals.
- Hybrid Care Models: Implementing hybrid models that combine in-person and telehealth services can help maximize accessibility while maintaining the benefits of face-to-face interactions.
- Cultural Sensitivity: Consider cultural factors that may influence students' willingness to seek mental health support, especially among non-English speaking or immigrant families.
- Further Research: Conduct qualitative studies to understand why distressed youth may not seek help and explore creative options like peer-to-peer support to address social isolation.
The Path Forward
The pandemic has highlighted the critical role SBHCs play in providing accessible mental health care to adolescents, particularly those from under-resourced communities. As we navigate the post-pandemic landscape, it is crucial for practitioners to adapt their approaches based on research findings and continue exploring innovative solutions to address the ongoing youth mental health crisis.
The Impact of School Closures on Service Utilization in School-Based Health Centers