The majority of persons with Alzheimer's disease (AD) live with a family member in the community. Among the challenges that AD introduces in a family, the most significant may be its impact on communication. Family members typically have a long history of interpersonal communication habits which they relied on prior to the onset of AD. When confronted with the changing cognitive and social behaviors of the person with AD, however, family members may not know that they could alter their own communication behavior to accommodate their loved one, and even if they do, they may not know how to accommodate effectively. To address this need for family care partner education and training, several communication-based programs have been developed and evaluated. In this article, we present a new program, Training in Communication Enhancement for Dementia (TRACED), that integrates two empirically, theoretically informed, and complementary approaches to enhancing communication in family care partnering contexts.
Specifically, TRACED combines principles of compensating for the cognitive and communication limitations of the person with AD alongside connecting with the person on a relational level by affirming, supporting, and enhancing the person's expression of self in everyday interactions, and recognizing the importance of family communication patterns. The TRACED training program ensures that compensatory strategies are practiced in meaningful person-supporting communication activities, and that connecting strategies are conveyed using appropriate accommodating behaviors. Following our presentation of TRACED, we report findings from a phase one pilot study that demonstrated the feasibility of TRACED and led to improvements in its content and delivery. Lastly, we consider how interventions such as TRACED could be made more accessible to families and other care partners in the community.
The Need for Family Communication Training in AD
Family members of persons with AD often have a long history of interacting with the affected person and have long-standing habits and patterns of interaction to which they give little or no thought until illness-related difficulties become evident. In addition, some family members have insights into their partners' communication needs and preferences but do not know how to use this knowledge effectively. Because dementia brings about considerable changes in cognitive and psychosocial functioning, family members may find that the communication skills and/or awareness they used to rely on are no longer adequate to meet the new challenges they face (Farran, Loukissa, Perraud, & Paun, 2003; Magai, Cohen, & Gomberg, 2002). Moreover, research has found that care partners' perceptions of how they communicate with a person who has AD do not always coincide with their actual communication behaviors (McCann, Gilley, Hebert, Beckett, & Evans, 1997; Small, Gutman, Makela, & Hillhouse, 2003), and that some of these behaviors are not conducive to positive communication outcomes (Orange, 1991; Orange, Lubinski, & Higginbotham, 1996; Perry & Small, 2006; Ripich, Ziol, Fritsch, & Durand, 1999; Small & Perry, 2005; Small et al., 2003).
Communication Strategies in TRACED
Several communication-focused training programs for AD care partners have been developed and evaluated. However, a recent systematic review of communication interventions for AD care partners revealed that there are very few investigations that have targeted family members who care for relatives with AD in their home (Zientz et al., 2007). Most focus the interventions on health care providers who have no personal history with the person with AD and rely instead on communication skills that are gained as part of professional education. Moreover, although Zientz et al. (2007) concluded that the findings from these studies generally support caregiver education and training in communication strategies for individuals with dementia (p. lxii), these and other authors have cautioned that there are theoretical and methodological limitations of this research which need to be addressed in future research (see also Byrne & Orange, 2005b).
The TRACED Program
The basic premise of the TRACED program is that both compensatory (cognitive-linguistic) and connecting (relational-psychosocial) dimensions must be addressed and practiced together in order to enhance communication. Focusing on only one dimension will significantly compromise the benefits of care partner communication training. The distinct innovation of TRACED is its integration of empirically-based compensatory and connecting strategies within well-recognized and accepted theoretical frameworks which incorporate both of these dimensions. Specifically, TRACED is based on:
- Care partner strategies that have been shown to be associated with positive communication outcomes, such as fewer communication breakdowns and more effective resolution of breakdowns, and supporting the self of the person with dementia and facilitating their participation in social interactions (Orange & Colton-Hudson, 1998; Orange, Van Gennep, Miller, & Johnson, 1998; Perry & Small, 2006; Perry & O'Connor, 2002; Small, Kemper & Lyons, 1997; Small & Perry, 2005; Small et al., 2003).
- Principles from communication accommodation and enhancement theories (Coupland, Coupland, Giles, & Henwood, 1988; Kemper, Anagnopoulos, Lyons, & Heberlein, 1994; Ryan, Giles, Bartolucci, & Henwood, 1986; Ryan, Meredith, MacLean, & Orange, 1995; Small, 2006).
Findings from the Pilot Study
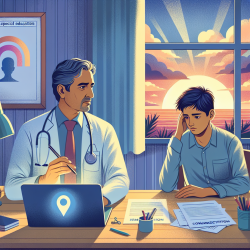
To assess the feasibility of implementing the TRACED protocol with family care partners, we conducted a phase one pilot study that offered six weekly training sessions to six care partners and their spouses with ADRD. There were two trainers with master's degrees in adult education, and/or gerontology and experience working with people with dementia and their families. Each trainer worked with different care partners and was accompanied by an assistant who engaged the spouse with dementia in meaningful activities while the care partner received training. In its original delivery, the TRACED program ran up to 2.5 hours in length. Feedback from care partners and trainers indicated that a more appropriate time frame would be 1.5 to 2 hours, which is the target length of the revised TRACED sessions. All participants spoke English as their primary language. Care partners' ages ranged from 59-73 years (M = 66 years), and spouses with AD from 64-81 years (M = 72). Years of education of care partners ranged from 11-18 (M = 14), and for spouses with AD from 9-22 (M = 15). Five spouses with AD were diagnosed with AD, and one with mixed dementia, and had MMSE scores ranging from 16-22 (M = 18). All were taking dementia medications (Aricept or Reminyl). One care partner and one spouse with dementia did not provide their education level, and MMSE scores were unavailable for two spouses with dementia.
Future Directions
Although follow-up research is warranted to examine the efficacy of TRACED, we believe the phase one findings and revisions of the protocol provide a foundation for adapting the TRACED training and manual for use by community service providers who work with families (e.g., home health care workers; hospital-based geriatric counseling and education outreach staff; cf. Young, Manthorp, Howells, & Tullo, 2011). In adapting TRACED for health care professionals, and others in clinics and assessment units, the teaching strategies would be modified to build on participants' knowledge of the communication process as learned in most health care education programs. Some factors to consider in adapting the TRACED protocol for community settings are: 1) the duration of training (i.e., there may need to be shorter and/or fewer training sessions to accommodate service provider time constraints); 2) the influence of the service provider's experience, personality, and training background on understanding and effectively delivering TRACED (e.g., the concepts and principles of TRACED may need to be elaborated on/simplified for persons who do not have background knowledge in these areas); and 3) methods to monitor efficiently and evaluate progress by the trainees (e.g., use of self-report and/or real-time observations). One approach to developing an adapted version of TRACED would be to consult with a variety of community service providers. This could take the form of focus group discussions, in order to identify their needs and constraints in implementing a program like TRACED. Actual training could then be implemented using a train-the-trainer approach so that key individuals from community agencies are trained on how to train their staff (e.g., Fitzgerald et al., 2009).
As an alternative to an in-person care partner training program, Smith et al. (2011) created an instructional DVD for family and institutional carers. The DVD content focuses on educating care partners on compensatory strategies to assist with memory function and facilitative strategies to help maintain communicative function (p. 261). In particular, it includes vignettes of scripted role acting, interactive opportunities for the viewer to consider the use or non-use of strategies in these vignettes, and commentary from a discipline specialist to highlight strategy use or non-use. Supplementing the video is a summary booklet which is intended to help either family or professional care partners retain and apply the content in their own caregiving experience. An obvious benefit of packaging a communication education program in DVD format is that it