Introduction
Hydrocephalus, a condition characterized by an accumulation of cerebrospinal fluid (CSF) in the brain, poses a significant challenge when it occurs in patients with leptomeningeal metastases (LM). This condition often arises as a complication of advanced cancer, severely impacting patients' quality of life. A recent research article titled "Management of hydrocephalus in patients with leptomeningeal metastases: an ethical approach to decision-making" delves into the complexities of managing this condition. This blog aims to guide practitioners in integrating ethical principles and patient-centered approaches into their clinical decision-making processes.
Management Options
The management of hydrocephalus in LM patients involves several options, each with its own set of benefits and risks:
- Shunt Placement: This involves inserting a catheter to divert CSF, providing symptomatic relief but also carrying risks such as infection and bleeding.
- Repeated Lumbar Punctures: While effective for acute symptom relief, they can be uncomfortable and impractical for long-term management.
- Intraventricular Reservoir Placement: Offers a less invasive alternative to repeated lumbar punctures but may still lead to complications like infection.
- Endoscopic Third Ventriculostomy (ETV): Suitable for obstructive hydrocephalus, ETV is less invasive than shunt placement but not always applicable.
- Non-Intervention: Focusing on pain management without surgical intervention may be preferred by some patients due to the poor prognosis.
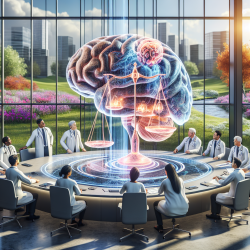
Ethical Considerations
Given the complex nature of LM-associated hydrocephalus, decision-making should extend beyond clinical considerations to include ethical principles:
- Respect for Autonomy: Physicians should honor the patient's values and choices, ensuring informed consent and decision-making capacity are prioritized.
- Non-Maleficence: Avoiding harm is crucial, requiring a balance between potential benefits and the risks of interventions.
- Beneficence: The aim is to maximize patient benefit, considering individual prognosis and treatment goals.
- Justice: Fairness in treatment decisions is essential, ensuring all patients receive comprehensive information and equitable care.
Patient-Centered Decision-Making
Effective management of hydrocephalus in LM requires a collaborative approach between the physician, patient, and their family. Practitioners should:
- Establish the patient's decision-making capacity early in the process.
- Provide clear, unbiased information about all management options and their potential outcomes.
- Incorporate the patient's values, cultural beliefs, and personal priorities into the decision-making process.
- Consider involving palliative care teams to align treatment with the patient's values and improve quality of life.
Conclusion
The management of hydrocephalus in patients with leptomeningeal metastases is a complex interplay of medical and ethical considerations. By integrating patient-centered approaches and ethical principles, practitioners can enhance the quality of life for these patients. For a more comprehensive understanding, I encourage you to read the original research paper, Management of hydrocephalus in patients with leptomeningeal metastases: an ethical approach to decision-making.