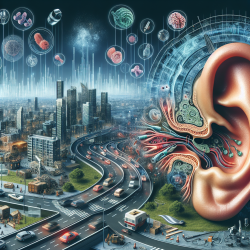
The prevalence of hearing impairment is a growing concern worldwide, affecting over 460 million individuals. Despite its significant impact, hearing loss remains underassessed in primary care settings. Recent advancements in serological biomarkers offer promising new approaches for early detection and understanding of hearing health issues. One such biomarker is prestin, a protein integral to the function of cochlear outer hair cells (OHCs). This blog explores recent research findings on prestin's role in predicting noise-induced hearing loss (NIHL) and discusses how practitioners can leverage these insights to enhance their practice.
The Role of Prestin in Hearing
Prestin is a motor protein crucial for the electromotility of OHCs, which amplifies sound vibrations within the cochlea. This amplification is vital for acute auditory sensitivity and effective communication. Damage or loss of OHCs can lead to significant hearing deficiencies, including NIHL and age-related hearing loss.
The study "Noise exposure levels predict blood levels of the inner ear protein prestin" investigates the relationship between environmental noise exposure and serum prestin levels. It highlights that individuals with higher routine noise exposure tend to have lower serum prestin levels. This finding suggests a potential link between noise exposure and subclinical OHC damage.
Key Findings and Implications
The research presents several hypotheses regarding the relationship between serum prestin levels and noise exposure:
- Hidden Outer Hair Cell Damage Hypothesis: Suggests that lower serum prestin levels may indicate subclinical OHC damage due to routine noise exposure. This damage might not be detectable through standard audiometric tests but could be reflected in serum prestin levels.
- Environmental Downregulation Hypothesis: Proposes that loud environments may lead to decreased need for cochlear amplification, causing downregulation of prestin expression as an adaptive response.
The study's findings support the notion that serum prestin could serve as an early marker for NIHL, offering a more sensitive measure than traditional audiometric tests. This has significant implications for practitioners aiming to detect and address hearing loss at earlier stages.
Practical Applications for Practitioners
The insights from this research can help practitioners improve their diagnostic capabilities and patient outcomes. Here are some practical applications:
- Incorporate Serological Testing: Consider integrating serological testing for prestin levels into routine assessments for patients exposed to high noise levels. This could aid in identifying at-risk individuals before clinical symptoms manifest.
- Promote Noise Protection Strategies: Educate patients about the importance of protecting their hearing from excessive noise exposure. Encourage the use of ear protection devices in noisy environments.
- Pursue Further Research: Engage in or support further research on serological biomarkers like prestin to enhance understanding and treatment of hearing disorders.
The Future of Hearing Health
The potential of serological biomarkers like prestin to revolutionize hearing health care is immense. By providing a more nuanced understanding of cochlear dynamics and damage, these biomarkers can lead to earlier interventions and better management of hearing loss.
The study discussed here underscores the need for continued exploration into the complex interactions between environmental factors and inner ear health. As our understanding deepens, practitioners will be better equipped to prevent and treat hearing impairments effectively.
Noise exposure levels predict blood levels of the inner ear protein prestin