Introduction
In the realm of pediatric therapy, understanding the complex interplay between neuropsychiatric changes and therapeutic interventions is crucial. The research article "Neuropsychiatric changes following penetrating head injury in children" provides profound insights into how such injuries can affect children's mental health and cognitive functions. By delving into these findings, practitioners can refine their approaches to therapy, ensuring more effective outcomes for young patients.
The Case Study: A Window into Neuropsychiatric Changes
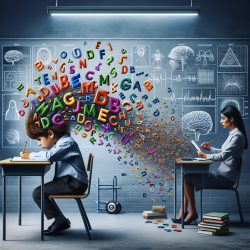
The research highlights the case of a 12-year-old boy who suffered a penetrating head injury, leading to significant neuropsychiatric changes. Initially diagnosed with bipolar disorder, the boy experienced a resolution of his symptoms post-injury, only to develop attention deficit hyperactivity disorder (ADHD). This case underscores the intricate relationship between brain injuries and psychiatric manifestations, emphasizing the need for a multidisciplinary approach in treatment.
Key Insights for Practitioners
For practitioners, the study offers several critical takeaways:
- Comprehensive Assessment: Post-injury, children should undergo thorough neuropsychological testing to identify deficits in executive functions such as attention, response inhibition, and processing speed.
- Monitoring Behavioral Changes: Continuous observation for behavioral shifts and new psychiatric disorders is essential. Early detection can lead to timely interventions, potentially mitigating long-term impacts.
- Interdisciplinary Collaboration: A collaborative approach involving neurology, psychiatry, and speech-language pathology can provide a holistic treatment plan, addressing both cognitive and behavioral aspects.
Implications for Speech-Language Pathologists
Speech-language pathologists play a pivotal role in the rehabilitation of children with brain injuries. By integrating the research findings into practice, they can tailor interventions to support cognitive and communicative functions effectively. Key strategies include:
- Targeted Therapy: Focus on enhancing attention, memory, and executive function skills through structured activities and exercises.
- Family Involvement: Engage families in the therapeutic process, providing them with strategies to support the child's communication and behavior at home.
- Adaptive Techniques: Utilize adaptive communication techniques and tools to facilitate learning and interaction, especially for children with processing speed deficits.
Encouraging Further Research
The case study also highlights the need for further research into the long-term neuropsychiatric outcomes of pediatric brain injuries. Practitioners are encouraged to contribute to this body of knowledge by documenting and sharing their observations and treatment outcomes. Such efforts can lead to more refined therapeutic approaches and improved quality of life for affected children.
Conclusion
The insights from the research on neuropsychiatric changes following penetrating head injuries in children provide a valuable framework for enhancing therapeutic practices. By embracing a data-driven approach and fostering interdisciplinary collaboration, practitioners can unlock the potential for better outcomes in pediatric therapy. To read the original research paper, please follow this link: Neuropsychiatric changes following penetrating head injury in children.