Understanding the Importance of Trained Interpreters in Informed Consent
In the realm of healthcare, informed consent is a cornerstone of ethical practice, ensuring that patients understand the procedures they undergo. However, for patients with Limited English Proficiency (LEP), achieving true informed consent can be challenging. A recent study titled "Are Good Intentions Good Enough?: Informed Consent Without Trained Interpreters" sheds light on the critical role trained interpreters play in bridging this gap.
The Study's Revelations
The study conducted by Hunt and de Voogd (2007) focused on prenatal genetics clinics in Texas, examining the informed consent process for Latina patients. It revealed that LEP patients often face significant disadvantages when untrained interpreters are used. The study highlighted four essential criteria for informed consent:
- Voluntariness: Patients must make decisions free from coercion.
- Discussion of Alternatives: Patients should be informed about all available options.
- Adequate Information: Patients need sufficient information to make informed choices.
- Competence: Patients must understand the information provided to make rational decisions.
Unfortunately, the study found that LEP patients consistently received lower informed consent scores compared to those who did not require an interpreter.
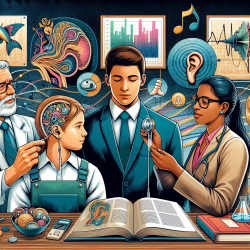
Why Trained Interpreters Matter
Trained interpreters are crucial in ensuring that the communication between healthcare providers and LEP patients is accurate, complete, and culturally appropriate. The study highlighted several issues with using untrained interpreters, such as:
- Inaccurate translations leading to misunderstandings.
- Omissions of critical information.
- Interpreters promoting their own agendas.
These issues can significantly impact a patient's ability to make informed decisions about their healthcare.
Implementing Change: Low-Cost Solutions
While hiring trained interpreters may seem costly, there are low-cost strategies that healthcare providers can implement to improve communication with LEP patients:
- Translating key documents, such as consent forms, into the patient's primary language.
- Testing staff for bilingual skills, particularly in medical terminology.
- Providing in-service training for staff to improve interpreting skills.
- Scheduling additional time for consultations that require interpretation.
These strategies can enhance the quality of communication and ensure that LEP patients receive the information they need to make informed healthcare decisions.
Encouraging Further Research
The findings of this study highlight the need for further research into the impact of language barriers on informed consent. Practitioners are encouraged to explore this topic further and consider the implementation of trained interpreters in their practice. By doing so, they can improve patient outcomes and uphold the ethical standards of informed consent.
To read the original research paper, please follow this link: Are Good Intentions Good Enough?: Informed Consent Without Trained Interpreters.