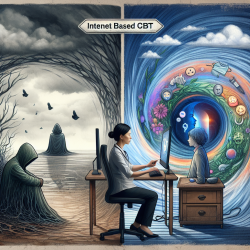
Early detection of psychotic-spectrum disorders among adolescents and young adults is critical for effective intervention. The initial years after the onset of psychotic symptoms represent a crucial period where psychosocial and pharmacological interventions are most beneficial. This blog summarizes key findings from the research article Identification of Psychosis Risk and Diagnosis of First-Episode Psychosis: Advice for Clinicians by Lundin et al. and offers actionable steps for practitioners to improve their diagnostic skills and outcomes for children and adolescents.
Understanding First-Episode Psychosis (FEP)
First-Episode Psychosis (FEP) refers to the initial occurrence of psychotic symptoms such as hallucinations, delusions, and disorganized speech. These symptoms can be highly distressing and disruptive. Identifying FEP early can significantly improve treatment outcomes. According to the research, the following symptoms are indicative of FEP:
- Frequent hallucinations or delusions
- Disorganized speech or behavior
- Severe functional impairment
Recognizing Psychosis-Risk Syndromes
Psychosis-risk syndromes, also known as Clinical High Risk for Psychosis (CHR-P), include early warning signs that indicate a heightened risk for developing a psychotic disorder. These signs can be subtle and varied, making early identification challenging. Key indicators include:
- Attenuated positive symptoms (e.g., unusual thought content, perceptual abnormalities)
- Brief intermittent psychotic symptoms
- Genetic risk factors combined with functional decline
Assessment Tools for Early Detection
Accurate assessment is essential for early intervention. The following tools are recommended for diagnosing psychosis-risk syndromes and FEP:
- Structured Interview for Psychosis-risk Syndromes (SIPS): Assesses psychosis-risk symptoms and syndromes.
- Comprehensive Assessment of At-Risk Mental States (CAARMS): Maps the onset of psychosis.
- Bonn Scale for the Assessment of Basic Symptoms (BSABS): Evaluates basic symptoms indicative of psychosis risk.
Differential Diagnosis
It is crucial to differentiate psychotic symptoms from other psychiatric conditions to provide appropriate care. Common conditions with overlapping symptoms include:
- Autism Spectrum Disorder (ASD): Social communication difficulties and sensory sensitivities can mimic psychotic symptoms.
- Obsessive-Compulsive Disorder (OCD): Intrusive thoughts and compulsions may resemble delusional beliefs.
- Post-Traumatic Stress Disorder (PTSD): Hypervigilance and flashbacks can be mistaken for paranoia and hallucinations.
Screening and Outreach
Effective screening and outreach are essential for early detection and intervention. Utilizing brief self-report assessments can help identify individuals at risk for psychosis. Outreach campaigns in schools, hospitals, and communities can facilitate early identification and referral to specialized care.
Conclusion
Early intervention in psychotic-spectrum disorders can significantly improve outcomes for youth. By utilizing evidence-based assessment tools and adopting a transdiagnostic approach, practitioners can enhance their diagnostic accuracy and provide timely, effective care.
To read the original research paper, please follow this link: Identification of Psychosis Risk and Diagnosis of First-Episode Psychosis: Advice for Clinicians