Anorexia of aging is a prevalent yet often overlooked condition affecting the elderly population. Characterized by a loss of appetite and reduced food intake, this syndrome can lead to undernutrition, unintended weight loss, and a decline in physical function. The recent study titled "Anorexia of aging: An international assessment of healthcare providers' knowledge and practice gaps" sheds light on the current challenges faced by healthcare providers (HCPs) in identifying and managing this condition.
Understanding the Knowledge Gaps
The study conducted an international assessment using a mixed-methods approach, including focus group interviews with subject matter experts and an electronic survey completed by 1,545 HCPs. The findings revealed significant knowledge gaps among practitioners:
- 56.8% of HCPs recognize a consistent definition of anorexia of aging as a loss of appetite or low food intake.
- Commonly identified risk factors include cognitive changes/dementia (91%) and dysphagia (87%).
- A significant number of respondents (38.7%) mistakenly believe that anorexia is a normal part of aging.
- Tools for screening appetite loss are underutilized, with only 39% using the Mini-Nutritional Assessment Short Form.
Enhancing Practitioner Skills
To address these gaps, practitioners can take several steps to improve their skills and patient outcomes:
1. Education and Awareness
Healthcare providers should engage in continuous education to stay informed about the latest research and best practices. Attending conferences, webinars, and workshops focused on geriatric nutrition can provide valuable insights into managing anorexia of aging effectively.
2. Comprehensive Assessment Tools
The study highlights the need for comprehensive assessment tools to evaluate appetite loss accurately. Practitioners should incorporate validated tools like the Mini-Nutritional Assessment Short Form into routine evaluations to identify at-risk individuals early.
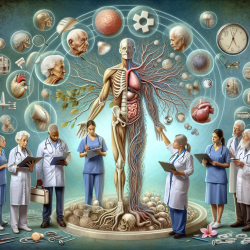
3. Collaborative Care Approach
A team-based approach involving dietitians, physicians, caregivers, and family members is crucial for effective management. Engaging caregivers in supporting older adults with anorexia can enhance adherence to nutritional and physical activity recommendations.
4. Addressing Misconceptions
Dispelling the myth that anorexia is a normal part of aging is essential. Educating both practitioners and patients about the condition's treatability can lead to more proactive management strategies.
Navigating Treatment Challenges
The study identifies treatment areas where practitioners can focus their efforts:
- Treatment is often centered on swallowing disorders (78%), dentition issues (76%), and increasing oral intake through fortified foods (75%) and oral nutritional supplements (74%).
- Lack of high-quality evidence is perceived as a barrier to optimal treatment (49.2%). Practitioners should advocate for more research in this area to develop evidence-based interventions.
Encouraging Further Research
The study underscores the importance of ongoing research to fill existing knowledge gaps. Practitioners are encouraged to participate in or support studies that explore innovative approaches to managing anorexia of aging. By contributing to research efforts, healthcare providers can play a pivotal role in advancing care for older adults.
To read the original research paper, please follow this link: Anorexia of aging: An international assessment of healthcare providers' knowledge and practice gaps.