Introduction
In the realm of military healthcare, musculoskeletal disorders represent a significant challenge, impacting operational readiness and resulting in substantial healthcare costs. The research article titled "Implementation interventions for musculoskeletal programs of care in the active military and barriers, facilitators, and outcomes of implementation: a scoping review" sheds light on the effectiveness of various implementation interventions aimed at improving care for musculoskeletal disorders in the military. This blog post explores the key findings of this research and how practitioners can leverage these insights to enhance their practice.
Understanding Implementation Interventions
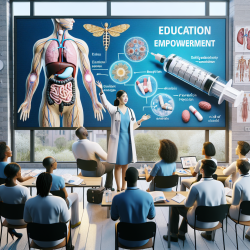
The scoping review identified several implementation interventions that have been used to deliver musculoskeletal care programs in the military. These interventions are primarily categorized under delivery arrangements and implementation strategies. The Effective Practice and Organization of Care (EPOC) taxonomy was utilized to classify these interventions, highlighting the importance of multidisciplinary care and coordinated healthcare delivery.
Multidisciplinary teams, often involving medical physicians, chiropractors, physical therapists, and psychologists, were found to be effective in managing musculoskeletal disorders. This approach facilitates coordinated care, early diagnosis, and aggressive reconditioning, bridging the gap between primary care and specialized treatment. Such interventions not only improve patient outcomes but also enhance the efficiency of healthcare delivery.
Barriers and Facilitators to Implementation
The research identified several barriers and facilitators to the implementation of musculoskeletal care programs. These were analyzed using the capability, opportunity, motivation-behavior (COM-B) system. Key barriers included a lack of formal training for support staff, limited access to necessary equipment, and high staff turnover, which necessitates repeated training.
Conversely, facilitators included the co-location of healthcare providers, which fosters communication and collaboration, and the presence of program champions who advocate for the implementation of evidence-based practices. Addressing these barriers and leveraging facilitators can significantly enhance the success of implementation efforts.
Outcomes of Implementation Interventions
The review highlighted that implementation interventions in the military setting have led to improved service and patient outcomes. These include enhanced efficiency in healthcare delivery, timely access to care, and improved patient satisfaction and symptomatology. Importantly, the implemented programs were found to be acceptable, appropriate, feasible, and sustainable.
These findings underscore the value of well-implemented multidisciplinary care models in achieving better health outcomes for military personnel. By focusing on implementation outcomes, practitioners can ensure that new treatments and services are effectively integrated into existing healthcare systems.
Future Directions and Research Implications
While the scoping review provides valuable insights, further research is needed to explore the optimal components of multidisciplinary care models. Questions remain about the ideal composition of healthcare teams, the necessity of co-location, and the specific roles of team members to maximize efficiency and effectiveness.
Additionally, future research should focus on developing reliable measures of implementation outcomes and exploring the effectiveness of behavior change techniques that address identified barriers. By advancing our understanding of these elements, we can enhance the implementation of musculoskeletal care programs and improve patient outcomes in the military.
Conclusion
Implementing effective musculoskeletal care programs in the military is crucial for maintaining operational readiness and improving patient outcomes. By understanding and addressing the barriers and facilitators to implementation, practitioners can enhance the delivery of care and ensure the sustainability of these programs. As we continue to explore the components of successful implementation interventions, we pave the way for improved healthcare delivery and better outcomes for military personnel.
To read the original research paper, please follow this link: Implementation interventions for musculoskeletal programs of care in the active military and barriers, facilitators, and outcomes of implementation: a scoping review.