Locked-In Syndrome (LIS) presents a unique challenge in the medical field due to its debilitating nature, characterized by severe motor impairment while maintaining cognitive function. As practitioners, enhancing communication for these patients is crucial to improving their quality of life. Recent advancements in technology and research provide promising avenues for facilitating effective communication with LIS patients. This blog post delves into these innovations and offers guidance for practitioners seeking to enhance their skills in working with this population.
Understanding Locked-In Syndrome
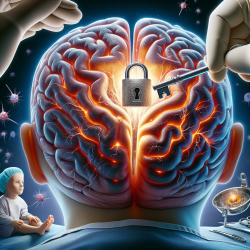
LIS is primarily caused by a vascular injury to the brainstem, often resulting from ischemia or hemorrhagic infarction. The condition leads to quadriplegia and anarthria while preserving awareness and ocular movements. Cognitive impairments can vary but often affect attention, memory, and higher-level functions. Establishing a functional communication system is vital for maintaining or improving the quality of life for LIS patients.
Communication Methods: From No-Tech to High-Tech
The spectrum of communication methods for LIS patients ranges from no-tech to high-tech solutions:
- No-Tech Solutions: These involve using bodily movements such as eye blinks or specific eye movements (e.g., up/down, right/left) to convey messages. This method requires both the patient and communication partner to understand the specific movements and their meanings.
- Low-Tech AAC: This includes tools like paper and pencil, letter boards, or simple voice output devices. For patients with preserved ocular movements, eye-gaze boards can be effective in selecting letters or words.
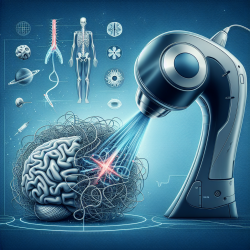
- High-Tech AAC: Advanced technologies like eye-gaze devices and brain-computer interfaces (BCIs) offer more sophisticated communication options. These tools allow patients to control electronic devices through neural signals or eye tracking.
The Role of Brain-Computer Interfaces (BCIs)
BCIs have emerged as a groundbreaking tool in facilitating communication for LIS patients. They translate neural signals into commands that can operate external devices, offering a direct link between the patient's brain activity and their ability to communicate. BCIs can be categorized into non-invasive and invasive types:
- Non-Invasive BCIs: These include technologies like electroencephalography (EEG) and functional near-infrared spectroscopy (fNIRS), which monitor brain activity without requiring surgical procedures. They offer a less risky option but may face challenges related to signal detection and interpretation.
- Invasive BCIs: Techniques such as electrocorticography (ECoG) involve implanting electrodes directly into the brain. While offering precise control over communication devices, they come with higher medical risks and ethical considerations.
Challenges and Considerations
While BCIs hold great promise, their implementation is not without challenges. Factors such as affordability, usability, access, and caregiver burden can impact their success. Practitioners must advocate for their patients to obtain necessary support and resources while considering each individual's unique circumstances.
The Path Forward
The field of AAC and BCI research is rapidly evolving, offering new opportunities to improve the lives of those affected by LIS. By staying informed about the latest developments and actively participating in ongoing research efforts, practitioners can play a pivotal role in advancing communication technologies for this population.
To read the original research paper that inspired these insights, please follow this link: Update on How to Approach a Patient with Locked-In Syndrome and Their Communication Ability.