The narrative review titled "Barriers and Mitigating Strategies to Healthcare Access in Indigenous Communities of Canada" offers crucial insights into the systemic challenges faced by Indigenous populations in accessing equitable healthcare. This comprehensive analysis categorizes barriers into proximal, intermediate, and distal levels, each requiring targeted strategies for mitigation.
Proximal Barriers: Immediate Challenges
- Geography: Remote locations often lack adequate healthcare facilities, necessitating travel for advanced care. Initiatives such as telehealth have been pivotal in bridging this gap.
- Education Attainment: Low educational levels can hinder the ability to navigate healthcare systems effectively. Programs aimed at improving education access are critical.
- Negative Bias: Stereotypes and biases among healthcare providers can lead to inadequate care. Cultural sensitivity training is essential for overcoming these biases.
- Staffing Shortages: Many communities face a shortage of qualified healthcare providers. Incentives and support programs can help retain staff in these areas.
Intermediate Barriers: Socioeconomic Factors
- Employment and Income: Economic disparities limit access to necessary health services. Investment in skills training and employment programs can alleviate these issues.
- Culturally Relevant Health Education: The lack of culturally competent curricula can deter Indigenous students from pursuing healthcare careers. Collaborative efforts with Indigenous communities are needed to reform educational systems.
Distal Barriers: Systemic Issues
- Colonialism: Historical policies have marginalized Indigenous communities, impacting current healthcare access. Collaborative governance models can foster reconciliation and inclusion.
- Racism and Social Exclusion: Systemic racism affects resource allocation and service delivery. Anti-racism policies and inclusive practices are vital for creating equitable healthcare environments.
Mitigation Strategies: Moving Forward
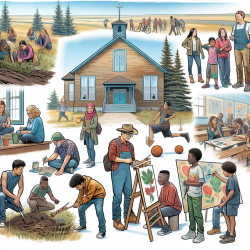
The review highlights several successful strategies implemented across Canada to address these barriers. These include financial investments in infrastructure, culturally sensitive education programs, and the involvement of Indigenous communities in policymaking processes. Practitioners are encouraged to engage with these strategies actively and consider further research to identify best practices for implementation.
The integration of traditional medicine with Western practices is another promising approach that respects cultural values while providing comprehensive care. Training programs that emphasize cultural competency can equip healthcare providers with the skills necessary to deliver respectful and effective services.
The Role of Practitioners
Healthcare practitioners play a crucial role in improving access and outcomes for Indigenous communities. By staying informed about ongoing challenges and participating in professional development opportunities focused on cultural competency, practitioners can enhance their ability to serve diverse populations effectively.
The narrative review serves as a call to action for practitioners to advocate for systemic changes that promote health equity. Engaging with Indigenous leaders and communities is essential for developing policies that reflect their needs and priorities.