Introduction
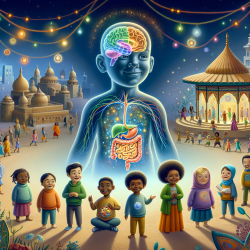
The field of psychogastroenterology has emerged as a crucial area of study that focuses on the intricate connection between the brain and the gut. This connection is particularly significant in children, where gut disorders often coincide with psychological and social factors that impact disease outcomes. As practitioners, understanding and implementing the findings from the research article "Psychogastroenterology: A Cure, Band-Aid, or Prevention?" can enhance our ability to improve pediatric outcomes.
Understanding the Brain-Gut Connection
The brain-gut axis is a bidirectional communication system that links the emotional and cognitive centers of the brain with peripheral intestinal functions. Recent studies have shown that psychological factors can influence gut health and vice versa. For instance, stress and anxiety can exacerbate gut symptoms, while gut microbiota can impact mood and behavior.
Traditional biomedical models often fall short in explaining these interactions, as they tend to separate mental health from physical health. However, the biopsychosocial model provides a more holistic approach by considering biological, psychological, and social factors in understanding health and disease.
Implementing the Biopsychosocial Model
To effectively address pediatric gut disorders, practitioners should adopt an integrative approach that combines medical and psychological care. This involves:
- Recognizing the role of psychological factors in gut health and vice versa.
- Incorporating psychological therapies that target gut-specific cognitions, emotions, and behaviors.
- Developing joint treatment plans with a multidisciplinary team, including psychologists, gastroenterologists, and dieticians.
By doing so, practitioners can provide comprehensive care that addresses both the physical and mental health needs of children with gut disorders.
Benefits of Integrative Care
Research has shown that integrative care models lead to better outcomes for pediatric patients. These benefits include:
- Reduction in gut symptoms and psychological distress.
- Increased patient and family satisfaction with treatment.
- Lower healthcare costs due to reduced need for extensive medical testing.
Furthermore, integrative care reduces stigma associated with mental health treatment, as it is presented as part of the overall management of gut disorders.
Conclusion
As practitioners, embracing the biopsychosocial model and integrating psychogastroenterology into our practice can significantly improve outcomes for children with gut disorders. By addressing both psychological and biological factors, we can provide holistic care that meets the diverse needs of our patients.
To read the original research paper, please follow this link: Psychogastroenterology: A Cure, Band-Aid, or Prevention?