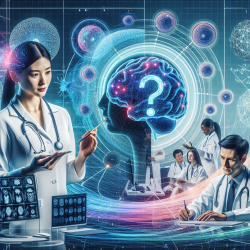
The preoperative assessment of patients undergoing intracranial surgery is a critical component of anesthesia practice. It involves a comprehensive evaluation of the patient's neurological condition, systemic health, and the specific requirements of the surgical procedure. This blog post explores key insights from the research article "Preoperative Assessment of Adult Patients for Intracranial Surgery" by Sivanaser and Manninen (2010), offering practical applications to enhance your skills in this area.
Understanding the Neurological Condition
A thorough understanding of the patient's neurological condition is essential. This includes reviewing their medical history, current symptoms, and any previous neurological events. Key considerations include:
- Neurological History: Documenting the type and location of lesions, symptoms such as seizures or raised intracranial pressure, and any neurological deficits.
- Neurological Examination: Assessing consciousness levels and conducting a detailed sensory and motor examination to evaluate cranial nerve function.
This comprehensive approach ensures that all potential complications are identified and managed appropriately during surgery.
Managing Systemic Health Conditions
The preoperative period is an opportunity to optimize systemic health conditions that could impact surgical outcomes. Key areas include:
- Cardiovascular Health: Identifying preexisting cardiac conditions and managing blood pressure fluctuations to prevent perioperative complications.
- Respiratory Health: Ensuring adequate oxygenation and ventilation by stabilizing any acute or chronic pulmonary conditions.
- Metabolic Conditions: Managing diabetes with tight glycemic control to reduce mortality risk in neurosurgical patients.
An integrated approach to managing these conditions can significantly improve patient safety and surgical outcomes.
The Role of Communication
An essential aspect of preoperative assessment is effective communication with both the patient and their family. This includes discussing:
- Anesthesia Techniques: Explaining the chosen anesthesia method and its implications for the procedure.
- Surgical Risks: Outlining potential risks associated with both the procedure and the patient's medical conditions.
- Postoperative Care Plans: Preparing patients for postoperative recovery requirements, including potential ventilation or pain management needs.
This dialogue helps set realistic expectations and fosters trust between the medical team and the patient.
The Importance of Multidisciplinary Collaboration
The complexity of neurosurgical procedures necessitates collaboration among various specialists. Engaging with neurosurgeons, neurologists, cardiologists, pulmonologists, and other relevant experts ensures a holistic approach to patient care. This collaboration aids in:
- Treatment Planning: Developing comprehensive plans that address all aspects of the patient's health.
- Surgical Preparation: Anticipating potential complications based on interdisciplinary insights.
- Crisis Management: Coordinating responses to intraoperative challenges effectively.
A multidisciplinary team approach enhances decision-making processes and improves patient outcomes.
Paving the Way for Further Research
The findings from this research highlight areas where further investigation could lead to improved practices in preoperative assessments for intracranial surgeries. Practitioners are encouraged to engage in ongoing education through conferences, publications, and webinars to stay abreast of advancements in this field. By doing so, they can continue to refine their skills and contribute to enhanced patient care standards.
If you're interested in delving deeper into this topic, I highly recommend reading the original research paper: Preoperative Assessment of Adult Patients for Intracranial Surgery.