The traditional view of placebos in clinical practice often revolves around deception—using them as a "lie that heals." However, recent research challenges this notion, suggesting that placebos can be a source of agency rather than deception. This shift opens new avenues for practitioners to enhance their skills and improve patient outcomes without compromising ethical standards.
The Power of Non-Deceptive Placebos
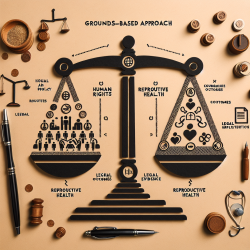
The research article "Placebos as a Source of Agency: Evidence and Implications" explores various mechanisms that contribute to placebo effects, such as classical conditioning, expectations, affective pathways, and open-label treatments. These mechanisms can be harnessed to bring about clinical benefits without deception.
- Classical Conditioning: This involves pairing two stimuli until one elicits the response typically produced by the other. For instance, conditioned responses have been documented in the immune system and can be used to taper medication dosages while maintaining efficacy.
- Expectations: Patient beliefs and verbal manipulations significantly impact placebo responses across various symptoms. By shaping expectations through positive narratives and supportive environments, practitioners can enhance treatment outcomes.
- Affective Pathways: The therapeutic alliance plays a crucial role in placebo responses. Empathy, warmth, and trust within the clinical encounter can lead to better patient outcomes.
- Open-Label Treatments: Even when patients are informed they are receiving placebos, significant improvements have been observed in conditions like IBS and chronic pain. This transparency respects patient autonomy while leveraging the placebo effect.
Implications for Clinical Practice
This new perspective on placebos encourages practitioners to view them as tools for enhancing patient agency rather than violating it. By understanding and utilizing non-deceptive placebo mechanisms, clinicians can foster a more collaborative and empowering therapeutic environment.
Acknowledging Limits: While placebos are effective for certain conditions like pain and mood disorders, they are not universally applicable. Practitioners must communicate these boundaries clearly to avoid misleading patients about the potential of placebo treatments.
Avoiding Blame: Emphasizing agency should not lead to blaming patients for their conditions. Instead, practitioners should focus on empowering patients through informed choices and supportive care.
Conclusion
The evolving understanding of placebos offers exciting opportunities for clinicians to enhance their practice ethically. By embracing non-deceptive methods, practitioners can improve patient outcomes while respecting autonomy and fostering trust.