Practitioners working with children and adolescents with chronic conditions face unique challenges, especially in low-income and middle-income countries (LMICs). The recent scoping review titled Models of lifelong care for children and adolescents with chronic conditions in low-income and middle-income countries: a scoping review offers valuable insights into effective care models that can guide practitioners in improving their skills and service delivery.
The Growing Need for Comprehensive Care
Non-communicable diseases (NCDs) or chronic conditions account for a significant portion of disability-adjusted life-years among young people under 20. This highlights the need for health systems to adapt and provide comprehensive care that extends beyond acute management. The review identifies common components of successful care models, including patient and family education, mental health support, and integration of community services.
Key Components of Effective Care Models
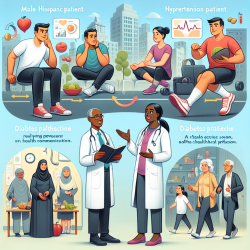
- Patient and Family Education: Educating patients and their families is crucial for disease self-management. This involves providing resources such as self-monitoring tools and training materials to empower families in managing the condition effectively.
- Mental Health Support: Addressing mental health is integral to managing chronic conditions. Incorporating social workers, psychologists, and peer support groups can enhance psychosocial well-being.
- Decentralized Services: Making healthcare accessible by decentralizing services from central hospitals to local clinics increases patient uptake and ensures regular follow-up.
- Differentiated Care: Tailoring care based on individual patient needs ensures that resources are used efficiently while providing appropriate levels of support.
Service Delivery Innovations
The review emphasizes the importance of flexible service delivery approaches. For example, using mobile technology for appointment reminders or consultations can improve adherence to treatment plans. Additionally, task-shifting—where less specialized workers are trained to handle routine care—can optimize healthcare resources.
Encouraging Further Research
The review highlights gaps in existing research, particularly the need for more diverse studies beyond HIV-focused models. Practitioners are encouraged to engage in implementation research to explore effective strategies for various chronic conditions. By contributing to this body of knowledge, practitioners can help develop scalable programs that address the growing burden of pediatric chronic diseases globally.
Implementing Research Findings in Practice
Practitioners can improve their skills by integrating these research findings into their practice. By focusing on comprehensive care that includes education, mental health support, and community integration, practitioners can enhance patient outcomes. Moreover, staying informed through continuous learning opportunities such as webinars or conferences will keep practitioners updated on best practices.
The full research paper provides a detailed analysis of these models and is a valuable resource for those looking to deepen their understanding of effective lifelong care strategies. To read the original research paper, please follow this link: Models of lifelong care for children and adolescents with chronic conditions in low-income and middle-income countries: a scoping review.