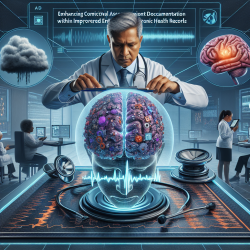
Introduction
The recent research article titled "Cognitive measures lacking in EHR prior to dementia or Alzheimer's disease diagnosis" by Maserejian et al. highlights a significant gap in the documentation of cognitive measures in electronic health records (EHR) before the diagnosis of dementia or Alzheimer's disease (AD). This gap poses challenges for timely diagnosis and quality care. As practitioners in the field of speech-language pathology and related healthcare professions, understanding and addressing these gaps can significantly enhance patient outcomes.
Key Findings from the Research
The study analyzed U.S. EHR data and found that only 11% of dementia patients and 24% of AD patients had a cognitive measure documented in the five years prior to diagnosis. Factors such as Black race, older age, non-commercial health insurance, and lower neighborhood income were associated with a lack of cognitive measures. This indicates that disparities in healthcare access and documentation exist, potentially affecting the quality of care and research.
Implications for Practitioners
For practitioners, these findings underscore the importance of implementing structured cognitive assessments and ensuring their documentation in EHRs. Here are some actionable steps:
- Incorporate Structured Cognitive Assessments: Utilize standardized cognitive assessments such as the Mini-Mental State Examination (MMSE) and ensure results are recorded in the EHR.
- Address Healthcare Disparities: Be proactive in assessing cognitive function in populations that are less likely to receive documented assessments, such as older adults and those from lower socioeconomic backgrounds.
- Enhance EHR Systems: Advocate for EHR systems that prompt cognitive assessments and facilitate the entry of results to improve data quality and accessibility.
Encouraging Further Research
While the study provides valuable insights, it also highlights the need for further research to explore the reasons behind the lack of cognitive data in EHRs. Understanding whether this is due to tests not being conducted, results not being entered, or EHR system limitations can guide interventions. Practitioners are encouraged to participate in or support research initiatives that aim to improve cognitive assessment documentation and address healthcare disparities.
Conclusion
Improving the documentation of cognitive measures in EHRs is crucial for timely dementia diagnosis and quality care. By addressing the gaps identified in the research, practitioners can contribute to better patient outcomes and advance the field of dementia care. For those interested in delving deeper into the study, the original research paper can be accessed through this link: Cognitive measures lacking in EHR prior to dementia or Alzheimer's disease diagnosis.